Designing an AR needle guidance system to safely and effectively aspirate fluid around the heart.
SUMMARY
As part of the Medventions Fellowship at Sunnybrook Hospital, I worked among an interdisciplinary team of engineers, med students and clinician leaders to develop a solution that combats a pressing need within cardiology. This experience was heavily guided by Stanford's Biodesign process and principles.
My Role: Engineer, Clinical Research
Timeline: Sept 2018 - Sept 2020
Tools Used: Slicer, Python, NDI Optical Motion Capture, SolidWorks, SLA 3D Printer, various machine shop tools
Note that some conceptual figures are hidden due to their proprietary nature.




PROBLEM
Pericardial effusion is a condition where there is excess fluid built up in the space surrounding the heart (the pericardium). In severe cases, this fluid can compress the heart and cause cardiac tamponade, a life-threatening emergency.
Treatment involves drainage of the pericardial sac to relieve pressure, however the current method involves a "best-guess" needle insertion based on a brief ultrasound image (i.e. clinician locates fluid via ultrasound, removes ultrasound, inserts needle in the approximate location of the fluid, then aspirates). This "best-guess" method is prone to error and while some cases it may be harmless, in others it can lead to emergency surgery (e.g. if a needle penetrates an artery).
SOLUTION
A plug-and-play AR needle guidance system that integrates motion capture, ultrasound and a virtual interface to safely aspirate fluid around the heart.
- The clinician first locates the fluid using an ultrasound and our system will mark its location in space.
- They can then insert the needle and with visual and haptic feedback, safely guide the needle to the target fluid location. If the clinician is off path, the system will beep to indicate a course-correction.
- Once they reach the target, the system will tell them it is safe to aspirate!
This solution eliminates the guesswork in pericardium fluid aspiration and minimizes preventable complications. A provisional patent was filed for this innovation.
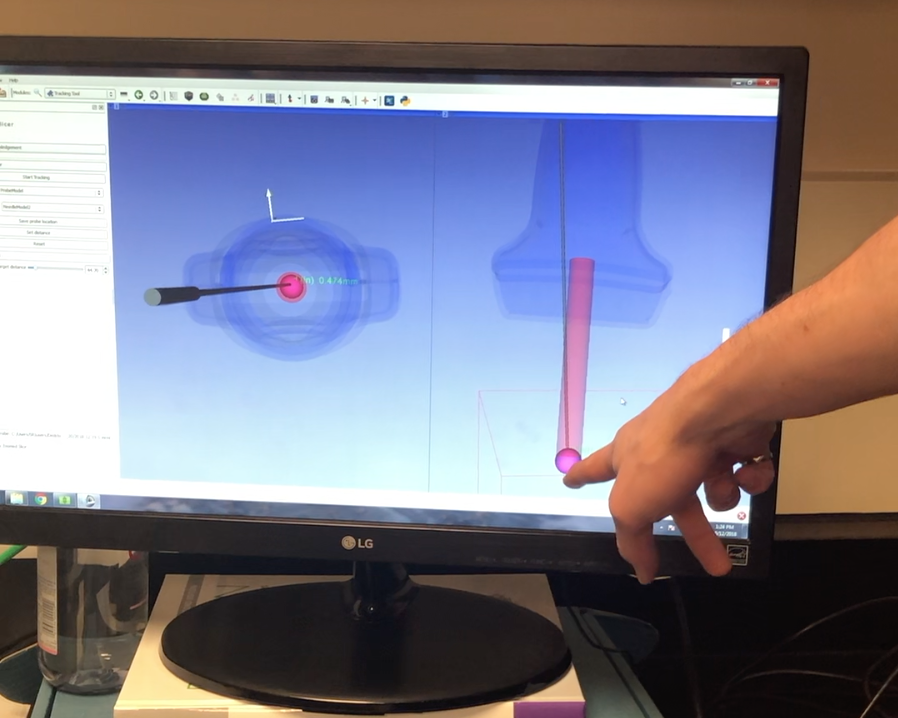
Screen capture of the AR system in use, where the needle is shown in grey, the guide path is shown by the red cylinder, and the target pericardial effusion location is the magenta sphere.
PROCESS & OUTCOMES
The Sunnybrook Medventions Fellowship spanned 4 months and was heavily influenced by Stanford's Biodesign process involving Stages 1) Needs Finding, 2) Needs Screening, 3) Concept Generation, and 4) Concept Selection.
The first 2 months were spent observing cardiology procedures, interviewing clinicians, nurses and admin staff to discover their biggest problems and largest needs. We gathered a list of 200+ needs and narrowed them down to the top 5 using an acceptance criteria matrix:
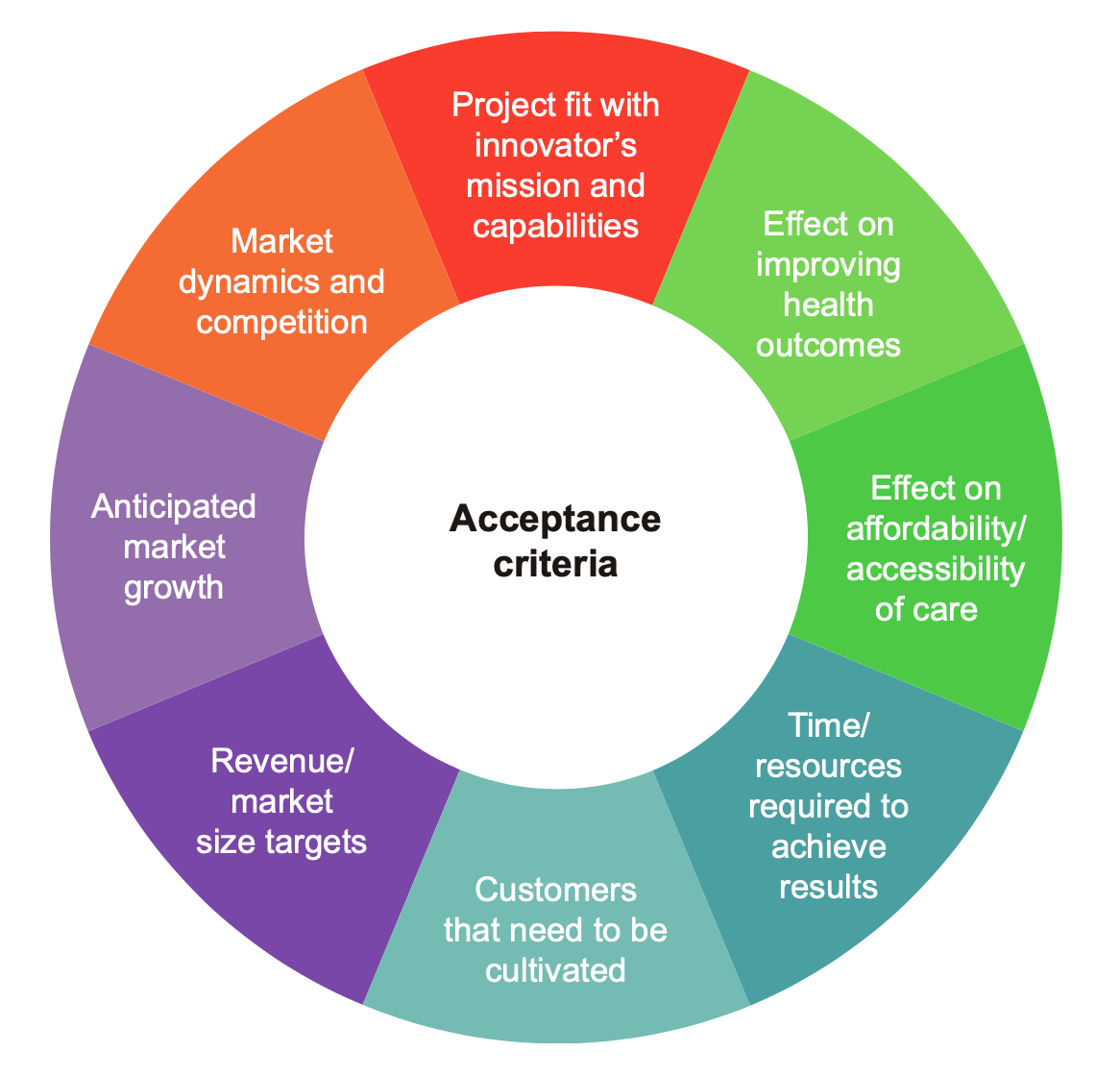
Acceptance criteria matrix from Stanford Biodesign Figure 1.1.3.
From this list of 5, we brainstormed potential concepts and more thoroughly evaluated their feasibility within the bounds of our skillset and timeline. This led us to choose a single solution, which we pursued alongside our partner Dr. Brian Courtney, a leading Sunnybrook Cardiologist, Scientist and Co-founder of Conavi Medical.
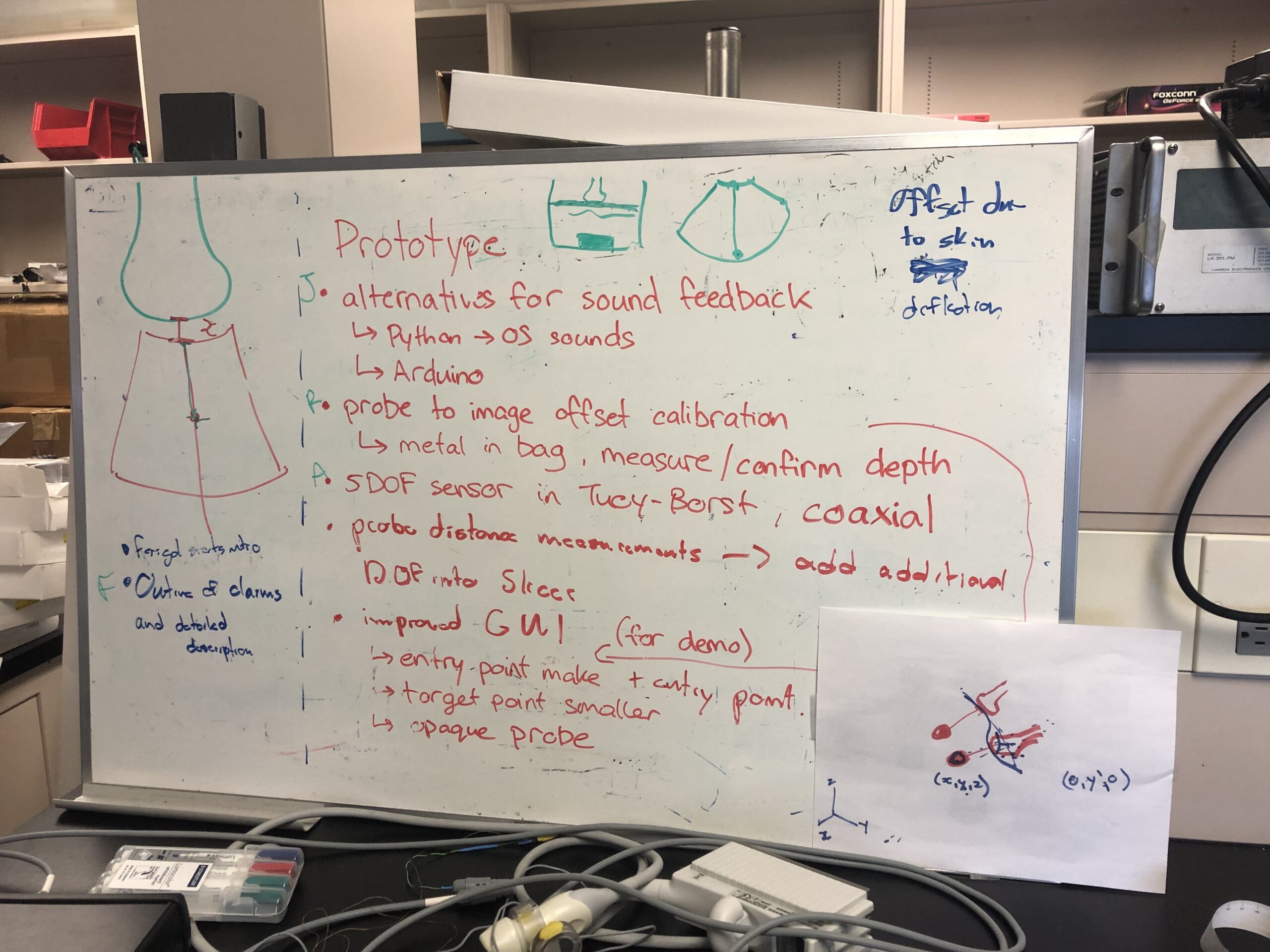
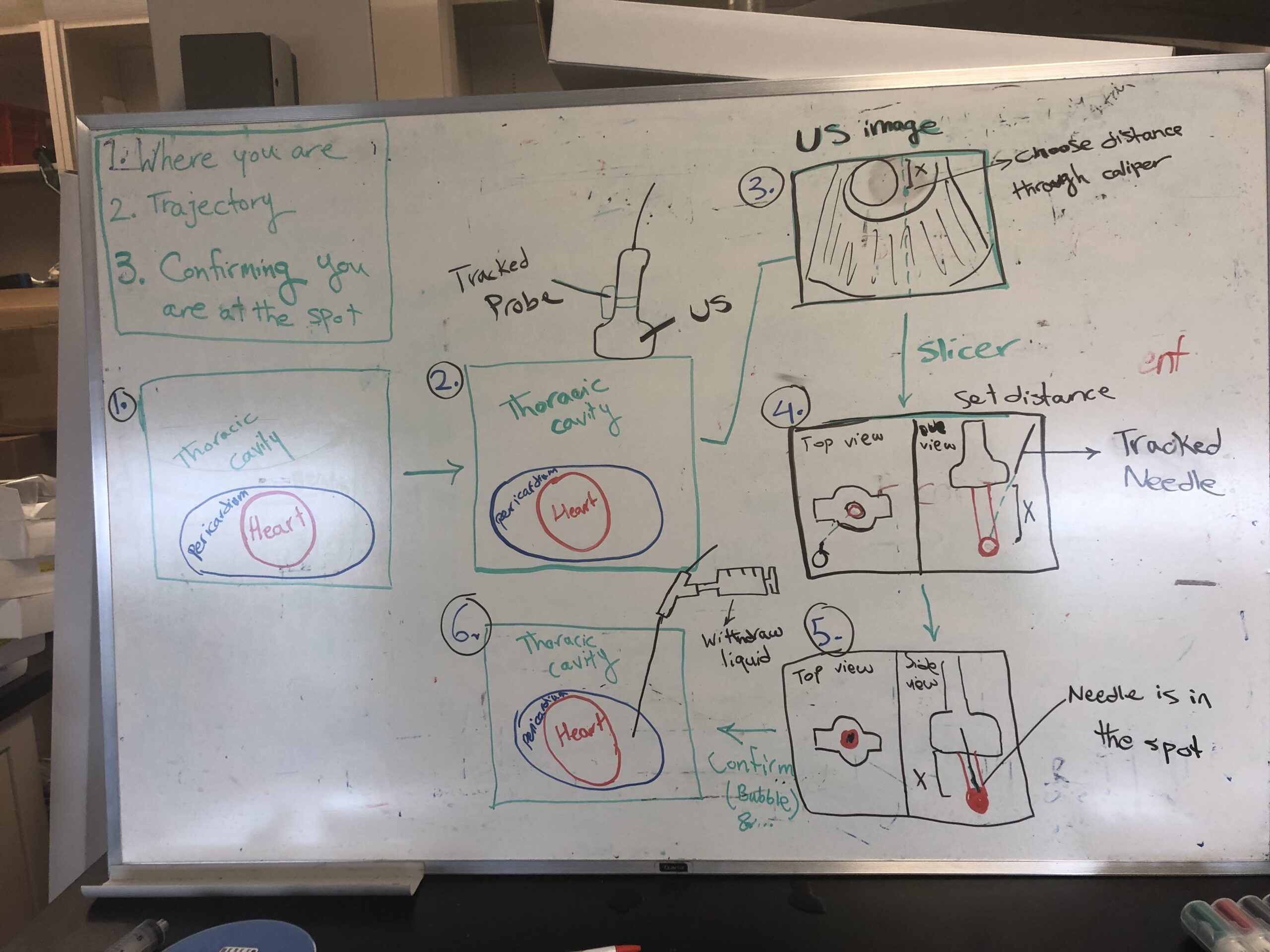
Brainstorming solutions & mapping out user flow
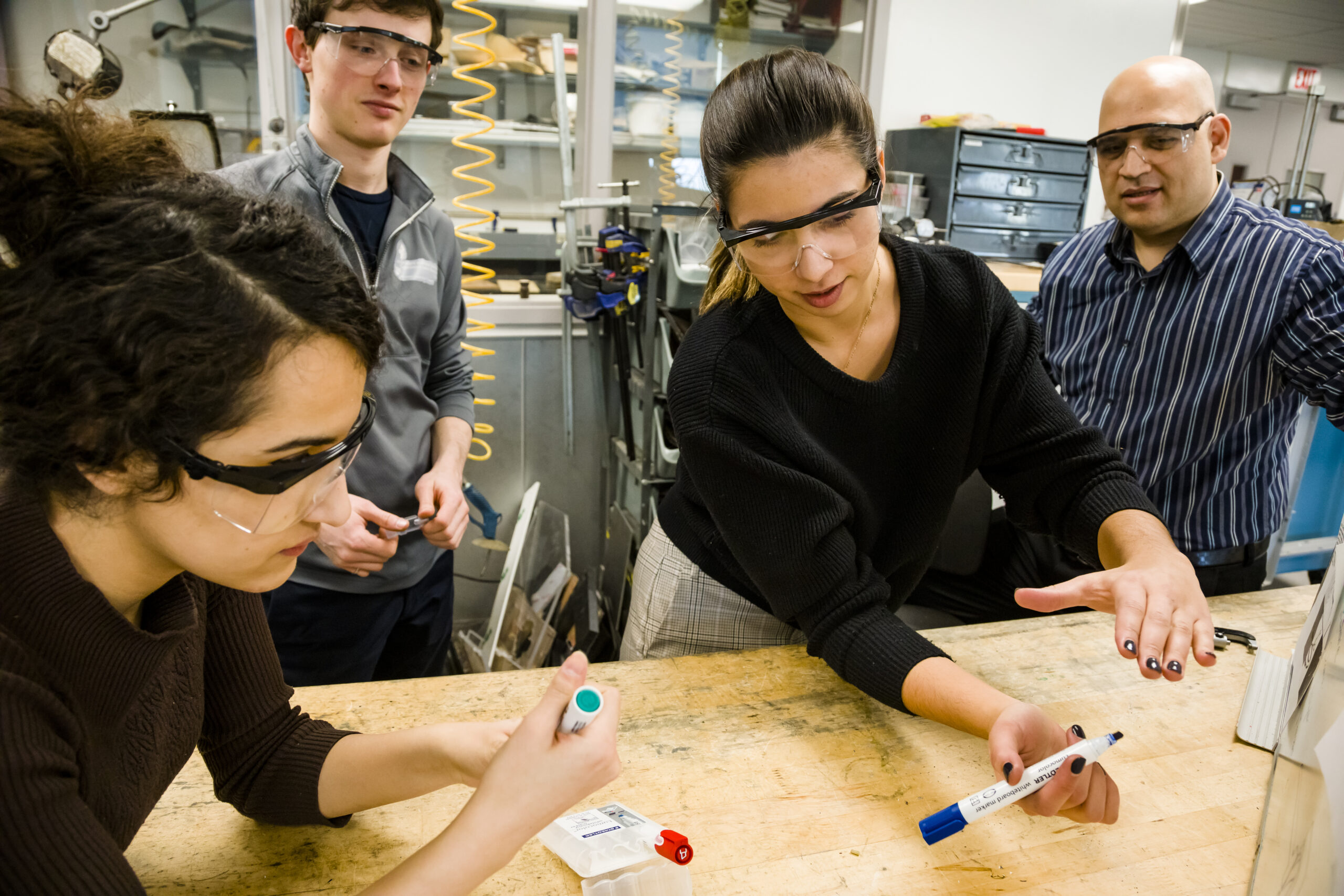
The final 2 months were spent designing and developing the solution, where we:
- Designed and 3D printed compatible mounts for the ultrasound and needle prototypes to integrate them with an NDI motion capture system.
- Used Slicer and Python code to create a visual interface showing the ultrasound and needle position and angle in space, and provide haptic feedback for needle entry.
- Created a heart phantom and fluid filled region using a silicone mold to simulate pericardial effusion.
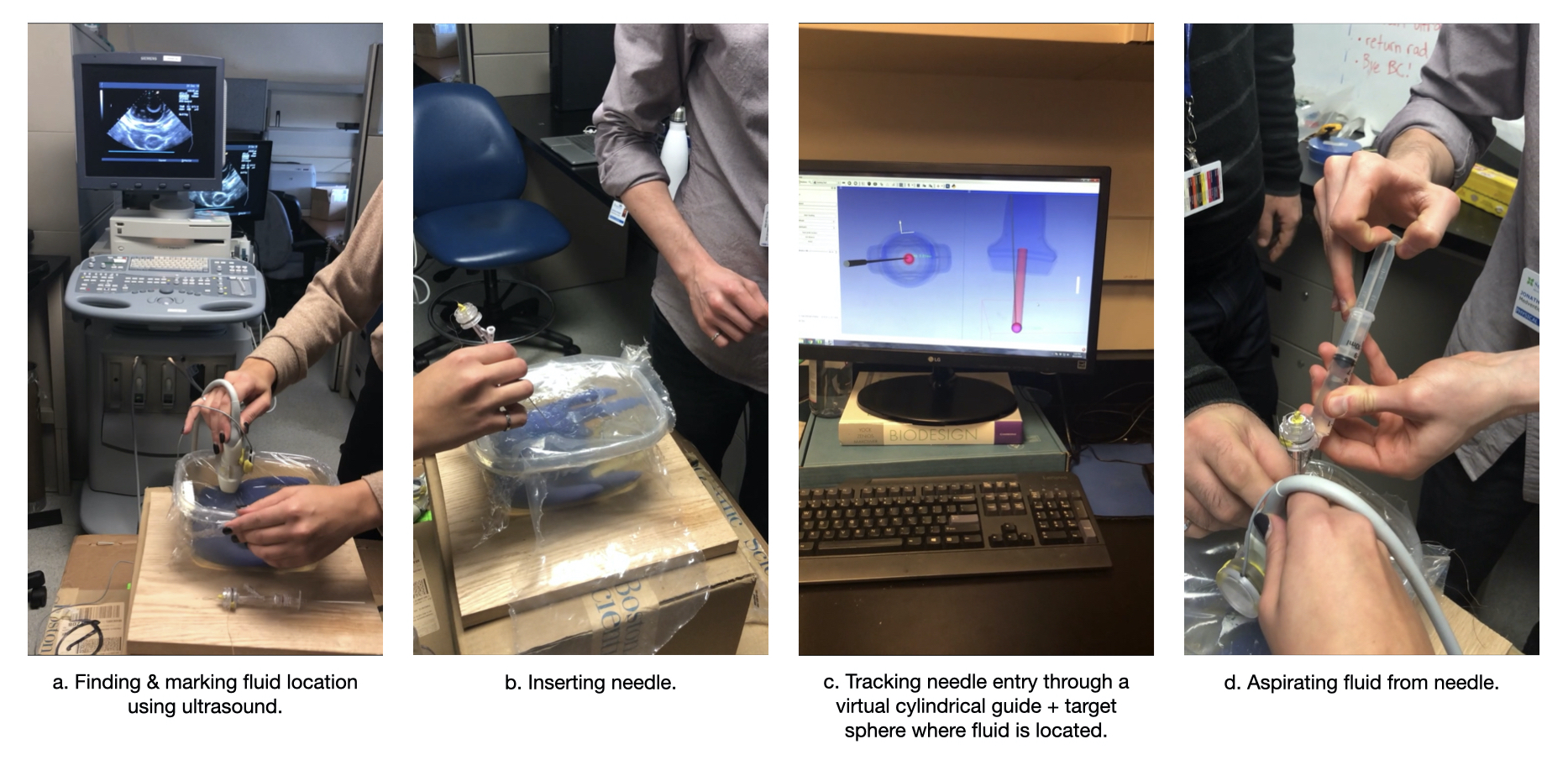
Once we were confident with a working prototype, we asked 5 residents and Dr. Courtney to test the solution and provide feedback. Based on this, we made improvements to the solution and determined that there was sufficient validation from users, interest from our partners and freedom to operate, to continue pursuing the solution beyond the fellowship.
As a team, we continued to develop a higher fidelity solution and filed for a provisional patent.
KEY TAKEAWAYS
1. Test Prototypes Early (Don't Wait to Perfect Your Solution)
My team had 2 months to generate concepts and build a solution; an extremely short amount of time. We worked diligently to create a working proof of concept prototype and had a round of user testing with only a couple weeks left. The findings from these tests were extremely valuable, for example: I designed a mount for the needle in the way that I intuitevly held it, only to realize that the operators hold it differently for this procedure. If this realization happened too late, it would have set us back a few weeks. Thus, it is extremely important to conduct user tests as early and often as possible in order to save time and resources down the line.
2. Prioritize Feasibility
The pursuit of this solution was highly dependent on what our team could accomplish during the fellowship period. If we had chosen a more complex idea, we would not have been able to build and test a prototype, let alone file a provisional patent. It was important that we pursued what was feasible given the constraints. This takeaway is applicable to all projects, physical or digital.
VIEW MY OTHER PROJECTS:
Xpan: A Less Invasive Surgical Access PortPhysical Products

Xpan Brand Revitalization: Logo & Web DesignDigital Products

New Start Foundation: Logo & Web DesignDigital Products

Fino: A Youth Financial Education AppDigital Products

100% Reusable Faceshields for COVID-19Physical Products